Prescribing medication in mental health clinics can be very complex.
The benefits from electronic prescribing (e-prescriptions) could be hugely significant, as there is a high risk to patients from existing paper prescription processes which is mitigated by the vigilance of the medical, admin and pharmacy staff.

Waiting room at outpatients' reception
Setting the scene
Mental health services have several different pathways for patients such as the Community Drug and Alcohol Team, Local Primary Mental Health Support Services, and the Community Mental Health Team (outpatients).
These teams include specialist mental health nurses and advanced nurse practitioners, some of whom are independent prescribers. There are also consultant psychiatrists who are available for specialist consultation, and for overseeing care across mental health teams.
The referral
Patients are referred into mental health services typically from a GP or acute and urgent services like CRISIS. GP referrals come through the Welsh Admin Portal (WAP), a GP system for referrals. Letters and emails are used for other referrals.
Screening and triage
Administrative staff print out the referrals from WAP and check the patient details on the various systems that could contain patient information, including:
-
Welsh Demographics System containing GP patient details and is used to check the patient's name, address, and characteristics
Electronic patient record systems include:
-
Welsh Patient Administration System (PAS) – used by clinics in both primary and secondary care
-
Care Partner – the primary electronic patient record system used by this clinic
-
Welsh Community Care Information System (WCCIS) – used for some patients who crossover into secondary care and who have key workers in social care
-
Carenotes
None of the electronic patient record systems currently being used has the ability to do e-prescribing.
The initial acceptance of a referral is an investigation because there is no one source of truth for patient information and their medical record, multiple sources have to be accessed and checked. Are they currently with an existing mental health team or have they ever been? Is the data we have on them correct? What medications are they on?
Keeping track of existing patients is also hard due to the various patient record systems in use by different teams – 4 in this clinic!
Consequently, once a week the Primary Care Admin Team Leader shares a printout of all the existing patients and which team or pathway they are in, as explained by the clinic lead:
Transcript:
A patient, for example, has got depression. At some point they might just need a primary care intervention, but at some point they might need quite a complex medication, then at some points they might be very unwell they need CMHT or crisis or inpatients, you know, it's the same person with the same disorder but depending where they are and how well they are, they might fit anywhere, they might move back and forth, so it's a fluid, they don't have a patient who's always in one service.
If they are a new referral, the patient is screened by a healthcare professional in clinic and directed to the correct pathway and triaged as urgent or not urgent. The patient has an account created on PAS and Care Partner (re-keying) and also on WCCIS if the patient requires multidisciplinary support.
The triage itself happens with the pathway team when a decision is made about how to handle the referral, and then an appointment is created and sent out.

A consultation room
Consulting, diagnosing, and prescribing
Prescriptions for most medicines are written, typed, or printed on paper WP10 forms, and are collected by the patient or, in some circumstances delivered to the pharmacy for the patient to collect there.
Prescriptions for some controlled drugs are written on CD80 forms, and these require a stricter process and governance.
Due to the risk associated with overdosing, most of the controlled drugs are prescribed daily, weekly, or fortnightly. One way to manage risk is to require daily dispensing from a prescription, where the patient is required to go to the pharmacy every day (when open), and the drugs are dispensed and then taken in the pharmacy and witnessed either by the pharmacist or key worker. Only some pharmacists will offer dispensing and observation of controlled drugs.
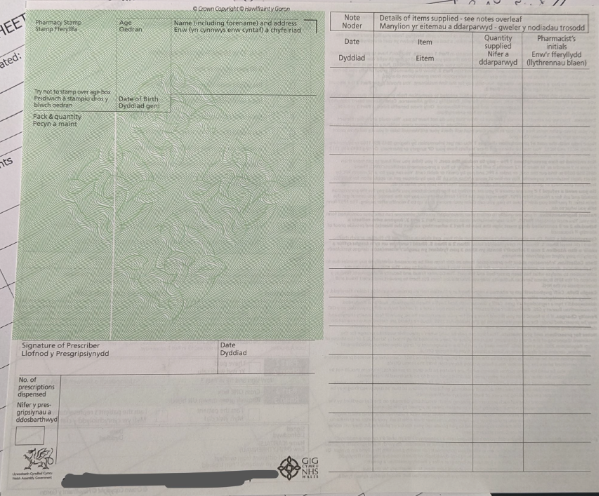
A prescription with a grid to log the frequency of dispensing, each time a dose is dispensed to the patient it would be signed by the pharmacist (and often the administration would be observed).
Once a prescription has been created the prescriber must:
-
update the notes in the various relevant electronic patient record systems (re-keying the information) usually with a scan of the prescription
-
send a letter (either in the post or email) to the GP with notes of medicine changes for them to attach to their GP records, which then get uploaded onto the Welsh Clinical Portal, yet another electronic patient record system that is accessible to most healthcare workers in both primary and secondary care. The quality of patient data is only as good as the weakest link in the system, and sometimes the note to the GP doesn’t get inputted onto the GP electronic patient record system by the surgery or their records are out-of-date posing a risk to the patient
Transcript:
Because if when I write on my letter that someone's taking something, they'll put it on, but for example I had a patient I reviewed yesterday, who actually, I was looking on Welsh Clinical Portal because of one of his GP prescriptions. So, he was telling me, I had my repeat protection from the GP and this was missing and because on portal, you can actually see what the GPs have issued and so I was like "Well, no, they have missed that off, haven't they? Okay I'll prescribe it for you so that you've got cover for that medication" but actually while I was on there, I noticed there are two or three things on there that they'd put as we were giving him and actually we hadn't given him for months, so if someone did that reconciliation at the hospital, for example and didn't have access to my notes which they wouldn't, they would think he was taking a bunch of things he's not taking.
Home visits mean that often the prescriber must take a photo of the prescription on their work phone and email that to themselves. The quality of the photo is often poor.
Scanning prescriptions involves scanning the paper document, which then gets emailed to the clinician, who then has to find and download the file and upload to the EPR(s). If the scanner breaks (not uncommon), then the system fails and there is no trail of the prescription other than what is written in notes, as the consultant explains:
Transcript:
Actually, I had a problem the other day when the stupid scanner broke and I scanned a bunch of them and thought they'd gone through because the way our scanner works is a Canon, so it scans it and it emails it to you, but at the computer you don't know that, it just says "yeah it's completed" and you're like "cool" and then you go back to your email and then I forward them or upload them or whatever and I got distracted from doing something else, I was in clinic, and then later I went "Oh okay, hang on, there's a bunch missing there that I'm sure I scanned some around that time" and they were on emails, but I saw the error message which was "Yeah sorry, there aren't any", I'd given them out already, so they're just not there, there's no record of those prescriptions now because I've already given them, the scanner broke, I didn't notice in time because I wouldn't, I would usually scan it and then go and give it to the patient and then go back to the clinic room, so I didn't notice.
Due to the number of electronic patient record systems in use by the clinic and different teams across the NHS where the patient may be being treated, prescribers are not always confident that they have the full picture of a patient’s medical record.

One of many printers in the clinic – a crucial piece of the ‘system architecture’ to enable prescriptions and data to be shared back to GPs and other EPR systems so other healthcare professionals can see what has been prescribed.
Multiple prescribers and prescriptions
It’s common for the patient to be under the care of more than one mental health specialist team and they could have a few different care plans.
As such, they could be getting multiple prescriptions from different prescribers.
Each of these prescriptions could be on a different frequency i.e., they could be required to be ordered and dispensed daily, weekly, fortnightly and the pharmacist will not collate the medicine so it can be dispensed together, as explained by the clinic consultant:
Transcript:
For example, if I have someone with ADHD who has a blister pack from their pharmacy, I can't do anything about that because I can't put my medication in that blister pack because my prescription is separate, so then you might have someone who's got complicated medication, I want to add something in but I can't do it because my prescription is not with that prescription.
Synching prescriptions to limit the number of visits the patient has to make to pick up their prescription from the clinic is a headache, as the consultant and admin lead explain:
Transcript:
We have some people who collect multiple times in a week, not necessarily daily, but just because of overdose risk, and you may have some patients with multiple medications on prescription pad, some are 16, some are 54, some, you know, 28 or whatever, so they are back and forth, nothing rings up then does it? And there are some times where we've started things kind of sequentially, we've seen those people ringing every week for a month for medication but they have all different prescriptions and so you try and do like "okay well let's, if we spot it, I'm like I'm sure I saw that name last week" and you try and get it all back into sync it's like "okay let me write enough, let me write two weeks of this one, three weeks of this one and four weeks of this one and then hopefully the next time it will be all together" but that's really difficult and again, another scenario is sometimes somebody will say "Well, I've struggled so I'll take two for a couple of days" then that prescription becomes earlier again, so again you try and get it all into sync, it's hard to actually monitor because any kind of audit involves you manually kicking through every one and double checking.
To limit the amount of administration, and to support the patient to have fewer collections and requests, clinicians will sometimes try to put patients with multiple prescriptions onto one prescription by ‘piggybacking’ on another prescription, asking that prescriber to put their medicine onto the prescription.
A consultant psychiatrist describes in more detail why they do this:
“I have to piggyback on the back of the CDAT prescription because someone might be getting prescriptions for different places, and they wouldn't add up timewise. So, their GP prescription will be available on one day, one week, and then CDAT is coming at a different time, and mine is coming at another time. So that person is managing multiple prescriptions at different times and requesting prescriptions at different times. And that's on top of all their own difficulties anyway.
People under our services don't tend to be very good with executive function commission because that's a big part of mental health and we’re asking a lot of people.”

The file of a key worker in the Drug and Alcohol Team containing prescriptions and notes.
Repeat prescriptions
There isn’t a way for non-GP clinicians to create repeat prescriptions.
If a patient has a condition which has stabilised to the point where a repeat prescription is appropriate, the specialist advanced practitioner nurse or consultant will request a shared or enhanced care agreement. GPs are not compelled to agree to this and in the case of mental health, many do not feel able to take on the responsibility and risk, so will refuse.
However, in repeat prescriptions, the mental health teams tend to manually write prescriptions every fortnight or month. Due to the amount of administration required, they are reluctant to issue them weekly, even though that might be better for the patient.
Keeping track of prescriptions
Knowing who has had what, when, is important to reduce the risk of overdose, as well as to combat potential fraud. However, it’s not easy to track prescriptions – it requires going into each patient record (on all the relevant patient record systems) and trawling through the notes and files.
This tracking of prescriptions is made harder by the fact that patients receiving mental health care move around from team to team, so there is no one person responsible for their continued care, making the quality and accessibility of patient data critical.
Example: A patient has got depression: they might need primary care intervention. But at some point, they might need quite a complex medication, and then, they might be very unwell and need to be seen by CMHT, crisis or inpatients.
Even though that person has the same disorder, it depends on where they are or how well they are, they might fit anywhere – they might move back and forth. So, it's fluid. You don't have a patient who's always in one service.
E-prescribing through the Electronic Prescription Service (EPS) could provide significant benefits for staff in reducing the admin burden or recording and sharing prescription information. However, the benefits would only result if the e-prescribing software were to replace existing patient record systems, rather than be an additional system for them to use.